ImPulse - A New Paradigm for Pediatric Cardiac Surgery Training

Useful information
- Team members
- Bashar Zapen
- Country
- Germany
- Keywords
- Surgical training heart surgery pediatric care simulation training 3D printing humanitarian design design thinking.
Short Description
ImPulse provides pediatric surgeons with an entirely 3D-printed baby & hearts for surgical training.
Detailed Description
ImPulse aims to establish a new paradigm for pediatric cardiac surgery training. Currently, the only way for trainee surgeons to practice pediatric surgery is to operate on actual patients. Unfortunately, this exposes patients to unnecessary risk; thus, senior surgeons hesitate to let trainees participate. Hence the need for simulation training modules that pose no threat to patients.
ImPulse offers trainees a high-fidelity simulation training module called Jan?n, simulating the various steps of pediatric cardiac surgery from start to finish in a safe environment that is accurate, consistent, repeatable, and uses the same tools and equipment as actual surgery.
Jan?n and its internal modules are 3D printable, with heart modules representing common congenital heart deformities that all pediatric cardiac surgeons should be able to treat. This is especially beneficial for economically and politically constrained areas where it is otherwise difficult to access medical training devices.
Project Details
- Does your design take social and cultural challenges and human wellbeing into consideration?
Congenital heart diseases are the most common form of birth deformities that require surgical intervention. Given the nature of infants, pediatric cardiac surgeons need to master their craft and develop advanced psychomotor skills to save such delicate yet complex organs. However, with its opportunity-based education, the current paradigm of surgical training programmes fails to provide trainees with adequate chances to develop those skills. Especially since they solely rely on actual patients for practising.
My research went through medical journals to identify the strengths and weaknesses of current surgical training programmes. Later I investigated emerging technologies in medicine, such as simulation training and 3D printing, that can accelerate the development of trainee surgeons’ skills. In addition, expert interviews were conducted with medical and humanitarian institutions to gain insight into Gaza’s pediatric cardiac services and existing training methods. Gaza was chosen due to my national origin [Palestine] and the region’s abnormally high prevalence of congenital heart diseases.
The interviews quickly revealed the dismal situation in Gaza, as no pediatric cardiac surgeries can be conducted locally due to the lack of infrastructure, materials, and pediatric surgery staff. As a result, pediatric patients with congenital heart diseases are referred to hospitals outside the region for treatment; around 30% of those referrals never get approval. Furthermore, according to personal correspondence and UN reports, the blockade on the Gaza Strip prevents crucial medical devices such as ultrasound machines and surgical training devices from entering. Hence, I needed to use local resources for my solution not to be affected by the blockade and to bypass it effectively. Fortunately, I found a local 3D printing facility through my correspondence with Forensic Architecture, thus giving me local means to produce and deliver my solution to Gaza’s medical universities and hospitals.
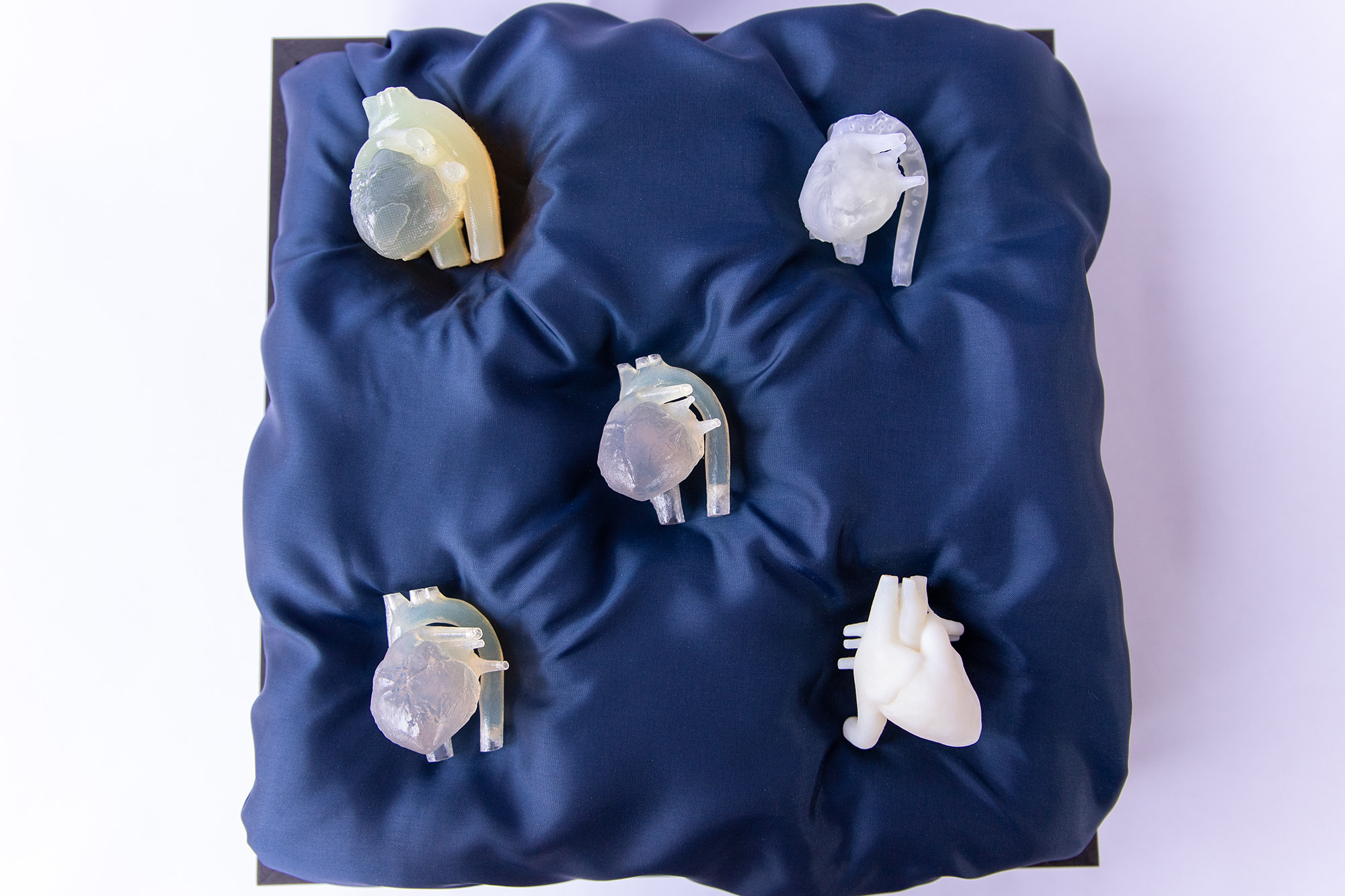
I designed Jan?n to be entirely 3D printable, with heart modules representing common congenital heart deformities that all pediatric cardiac surgeons should be able to treat. I developed the modules that address Gaza’s needs by taking actual patients’ CT scans and converting them into 3D models, which I later processed to be 3D printable. I then sculpted the congenital heart diseases in those models under the guidance of cardiac surgeons, maintaining anatomical fidelity. While the flexible 3D printed material makes it possible to operate on the hearts, I’m currently developing a new method to create the heart modules out of silicone to reduce costs and scale up production significantly.
- Does your design use principles of distribution and open source?
I made sure to use open-source and free software such as Blender, Meshmixer, and democratiz3D to convert and process CT scans into the heart modules in my project. I later 3D printed the heart modules in a flexible material that mimics the haptics of natural tissue, which can be cut and stitched like natural heart tissue.
Using the same design process and tools, it is possible to 3D print heart modules based on a specific patient's CT scans, allowing surgeons to rehearse novel procedures that would otherwise pose a significant risk to live patients. This makes Jan?n customisable to fit trainee surgeons’ needs and wants and usable for other training programmes besides pediatric cardiology.
Jan?n is entirely 3D printable, making it possible to create high-fidelity and high-resolution simulation training modules in constrained areas that would otherwise have no access to specialised fabrication machines or the ability to purchase/import simulation training devices.
I plan to clinically test Jan?n with my cardiac surgeon contacts in Germany and Tel-Aviv before sending the files to such constrained areas. In addition, all the design files and assembly manuals will be freely published online (probably through GitHub) to help surgical trainees worldwide develop their skills.
- Does your design promote awareness of responsible design and consumption?
Existing training programmes are not feasible to implement in politically and economically constrained areas, making it impossible to establish highly specialised and well-trained local surgical teams. So, I felt responsible to tackles the question of surgical training within the limits of those constraints while providing an unprecedented level of surgical simulation training and anatomical fidelity.
ImPulse aims to incorporate an easy-to-implement surgical training module [Jan?n] into pediatric cardiac surgery training programmes by utilising existing digital imaging devices and 3D printers. Operating on Jan?n enhances surgical trainees' psychomotor skills in a consistent and meaningful way, thus eliminating the reliance on low-risk patient cases for hands-on training. Trainees can then develop their skills on demand rather than when the opportunity arises. This is especially advantageous during times such as the pandemic, where practising on live patients is difficult, and mass distribution of simulation training devices is impossible.
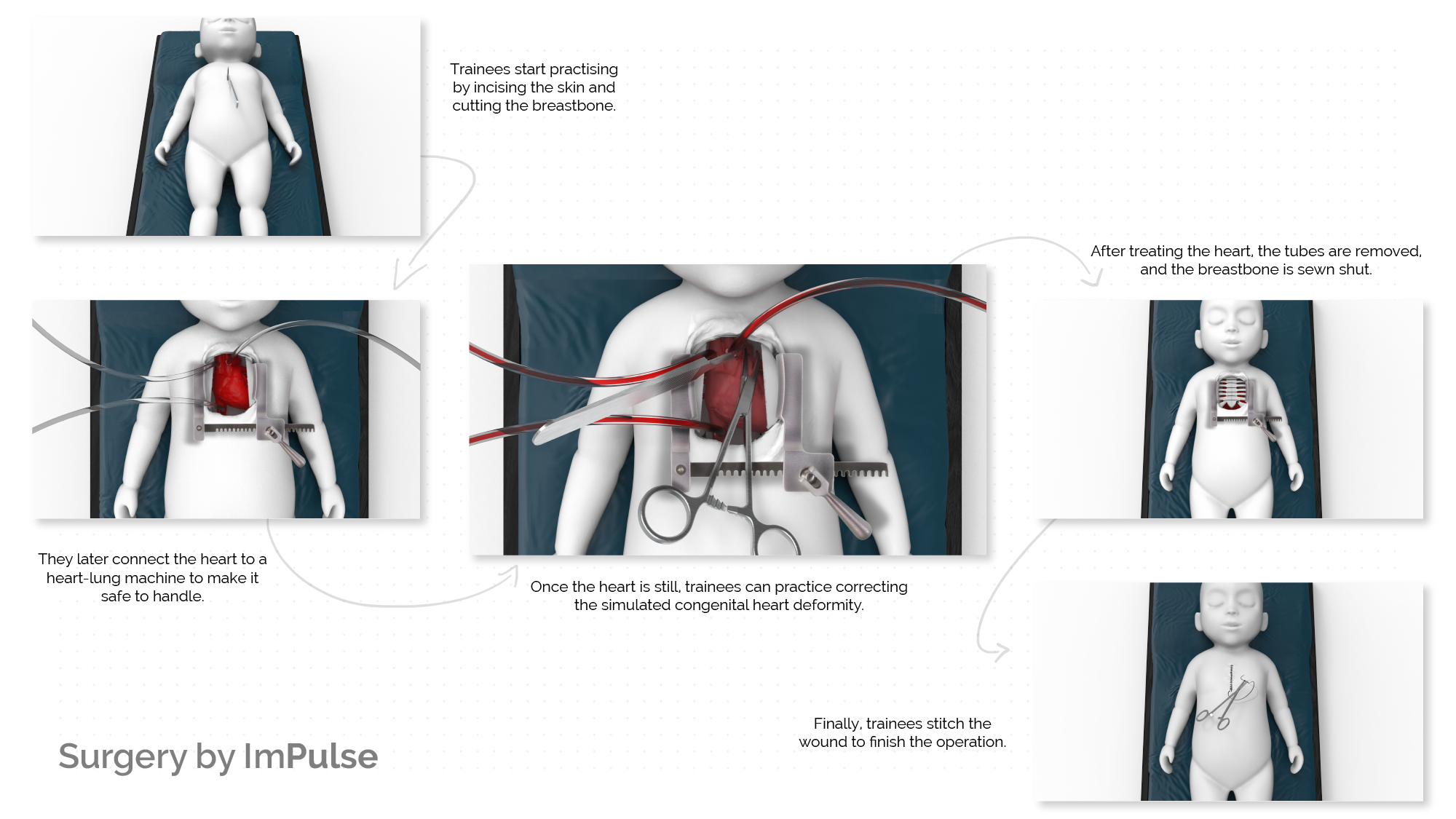
Unlike traditional ways of training, trainees can repeatedly practice congenital heart surgery from start to finish with Jan?n, giving them familiarity and confidence with all steps of the operation. For instance, trainees can cut open and stitch the chest and breastbone, connect the heart to a heart-lung machine (the basis of every open-heart surgery), and perform corrective surgery on the same module. In addition, Jan?n's modularity makes it easy to reuse, repair and replace components as needed and expands the number of surgeries possible.
Designers can solve our generation's pressing political, humanitarian, and ecological issues by being empathetic, inventive, collaborative, and resourceful. Personally, I'm using design to help establish the first pediatric cardiac surgery team in Gaza with my project, ImPulse, and Jan?n is my first step toward that goal.
Images